Foot Orthotics
Orthotics are shoe inserts that are meant to correct an irregular walking gait or provide cushioning to the feet. Orthotics come in a variety of different models and sizes, including over-the-counter and customizable variants. Customizable orthotics can be shaped and contoured to fit inside a specific shoe and are typically prescribed through a podiatrist who specializes in customized footwear and orthotics design and management.
Orthotics are beneficial because they can help prevent injuries from occurring and provide cushioning to keep pain levels down to a minimum. They also allow for the correct positioning of the feet. Orthotics can act as shock absorbers to help remove pressure from the foot and ankle. Therefore, orthotics can make bodily movements, such as walking and running, become more comfortable as well as help prevent the development of certain foot conditions.
Orthotics alleviate pain and make the foot more comfortable by slightly altering the angle at which the foot strikes the ground surface, therefore controlling the movement of the foot and ankle. Orthotics come in different variants and can be made of various materials. To determine what type of orthotic is most suited to your feet and your needs, it is best to consult your podiatrist. He or she will be able to recommend a type of orthotic that can help improve your foot function or prescribe a custom orthotic to best fit your feet.
Get Proper Care for a Sports-Related Foot or Ankle Injury This Fall
What is Joint Replacement Surgery?

Joint replacement surgery is a procedure that involves the removal of damaged or diseased portions of a joint and their replacement with artificial components. This surgery becomes necessary when joints deteriorate due to factors like arthritis, prolonged wear and tear, or underlying medical conditions. The primary objectives of foot or ankle joint replacement surgery are to alleviate pain, enhance joint functionality, and improve mobility. Before considering such surgery, podiatrists typically explore alternative treatments, such as exercise regimens, walking aids like canes or walkers, physical therapy, and medications to manage pain and inflammation. While joint replacement surgery can significantly improve a patient's quality of life, it is not without risks. Potential complications include postoperative infections, blood clot formation, and the eventual erosion of the artificial joint surface, which may require revision surgery after 15 to 20 years. If you are experiencing foot or ankle joint issues that have not responded to more conservative treatment, it is suggested that you make an appointment with a podiatrist to discuss whether joint replacement surgery is a viable treatment option for you.
In certain cases, in which the patient suffers from extreme pain or damage in a joint, joint replacement surgery may be deemed useful. If you have constant pain in a foot joint, consult with Edward Sharrer, DPM from Premier Foot and Ankle Clinic. Our podiatrist will assess your condition and provide you with quality foot and ankle treatment.
What Is Joint Replacement Surgery?
Over time, joints wear down; this can be exacerbated by diseases and conditions. Joint replacement surgery, also known as arthroplasty, is when a damaged joint is surgically removed and replaced with a prosthesis. Prostheses, which can be made of ceramic, plastic, or metal, act as joints in lieu of an actual joint. One of the most prevalent causes for joint replacement is arthritis.
Arthritis in the Foot
Arthritis can occur in any joint in the body, including in the feet. Common types of arthritis in the foot are osteoarthritis, rheumatoid arthritis, and gout. The big toe is usually where arthritis occurs in the foot; this is known as hallux rigidus.
Joint Replacement Surgery in the Foot
The most common form of joint replacement in the foot is a first metatarsophalangeal (MTP) joint placement. MTP joint replacement surgery is designed to treat hallux rigidus. Surgery is not intensive, and recovery occurs within one to two months after the procedure has been done. Overall, joint replacement surgery is a safe and effective way to treat pain in the joint of the foot.
If you have any questions, please feel free to contact our office located in North Little Rock, AZ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Joint Replacement Surgery
When conservative, noninvasive treatments prove unsuccessful, podiatrists will often turn to surgery as the last line of treatment for their patients. If patients are suffering from joint pain, issues in mobility, or are seeking to correct a deformity, joint replacement surgery is an effective option. Joint replacement surgery is also successful in treating arthritis, which is the most common cause of improperly working joints.
Patients with symptoms that include joint pain, stiffness, limping, muscle weakness, limited motion, and swelling are typically considered for joint replacement surgery. Range of motion and activity post-surgery will vary between patients and depending on the specific surgery performed, the affected joint, and the damage that will need to be repaired.
Joint replacement surgery replaces the damaged cartilage and bone, the latter if required. The damaged cartilage is typically replaced with a prosthesis that is attached to the bone, allowing the implant to grow into the bone. Following surgery, the patient will typically undergo physical therapy to become familiar with movement using the replaced joint.
Different Types of Foot Arthritis

Arthritis is characterized by inflammation in one or more joints, leading to pain and stiffness. It is prevalent in the small joints of the foot and ankle, impacting mobility and daily activities. While there is no cure for arthritis, treatment options can help manage symptoms and slow disease progression. The foot and ankle play vital roles in supporting, balancing, and absorbing shock during activities. These areas contain multiple joints and are susceptible to various forms of arthritis like osteoarthritis, rheumatoid arthritis, and gout. Osteoarthritis gradually erodes joint cartilage, causing pain, stiffness, and bone spurs. Risk factors include age, obesity, genetics, and poor foot alignment. Rheumatoid arthritis is a chronic autoimmune disease that can start in the foot and ankle, leading to joint inflammation, swelling, and deformity. Genetic and environmental factors can trigger this condition. Gout is a painful inflammation that often affects the big toe joint due to the accumulation of uric acid crystals. It can lead to sudden and severe joint pain. If you have foot or ankle discomfort from arthritis, it is suggested that you make an appointment with a podiatrist to determine which kind of arthritis is affecting you.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact Edward Sharrer, DPM from Premier Foot and Ankle Clinic. Our podiatrist can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a joint disorder that involves the inflammation of different joints in your body, such as those in your feet. Arthritis is often caused by a degenerative joint disease and causes mild to severe pain in all affected areas. In addition to this, swelling and stiffness in the affected joints can also be a common symptom of arthritis.
In many cases, wearing ill-fitting shoes can worsen the effects and pain of arthritis. Wearing shoes that have a lower heel and extra room can help your feet feel more comfortable. In cases of rheumatoid arthritis, the arch in your foot may become problematic. Buying shoes with proper arch support that contour to your feet can help immensely.
Alleviating Arthritic Pain
- Exercises that stretch the foot can prevent further pain and injury and increase mobility
- Most of the pain can be alleviated with anti-inflammatory drugs, heat, and topical medications
- Massages can help temporarily alleviate pain.
It is best to see your doctor for the treatment that is right for your needs and symptoms. Conditions vary, and a podiatrist can help you determine the right method of care for your feet.
If you have any questions, please feel free to contact our office located in North Little Rock, AZ . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Arthritic Foot Care
During your lifetime, you will probably walk about 75,000 miles, which is quite a lot of stress to put on your feet. As you get older, the 26 bones and 30 joints in each of your feet will lose flexibility and elasticity. Your foot’s natural shock absorbers will wear down as well. Having arthritis added to this mix only makes matters worse. Your joints will become distorted and inflamed, which is why arthritic foot care needs to be something to think about every day.
When dealing with arthritis, having additional foot complications, such as bunions, hammertoes, or neuroma, can be a serious detriment. To avoid these, buy well-fitting shoes with a lower heel and good support. Arthritis causes you to lose your arch, so having shoes with good arch support is also highly recommended.
Aside from getting good arch support, the shoes need to fit comfortably and properly as well. A good place to start is by leaving a finger width between the back of the shoe and your foot to gauge proper size. It is also helpful to have a square or rounded toe box in the front to provide even more comfort. Another thing to look for is a rubber sole that can provide a cushion and absorb shock as you walk. This adds flexibility to the ball of your foot when you push off your heel to walk.
Exercise is another key aspect of arthritic foot care. Exercise not only strengthens and stretches your muscles and joints, but helps to prevent further injury and pain as well. Stretching the Achilles tendon, the tendon located in the back of your heel, will give you added mobility and reduce pain due to stress. Another thing you can do is massage your feet, kneading the ball of your foot as well as your toes from top to bottom.
Stretching the Achilles tendon is a simple exercise that you can do at home anytime. Lean against the wall with your palms flat against the surface while placing one foot forward, towards the wall, and one foot behind you. Bend your forward knee towards the wall while keeping your back knee locked straight, and make sure both your heels are completely touching the ground at all times. This will stretch your Achilles tendon and calf muscles as well. You will feel the stretch almost immediately. You can also stretch your toes in a couple ways. One involves taking a rubber band and wrapping it around both your big toes while your heels remain together. Then, pull them apart to stretch your big toe. You can also place a rubber band around all the toes of one of your feet. Then, try to separate each individual toe, stretching them all.
A final step you can take to help your arthritis is taking non-steroid, non-inflammatory drugs or topical medicines with capsaicin. Unfortunately, there is no complete way to remove all of your arthritic pain. However, following some of this advice can go a long way in staying as pain-free as possible.
Getting Help for Plantar Fasciitis
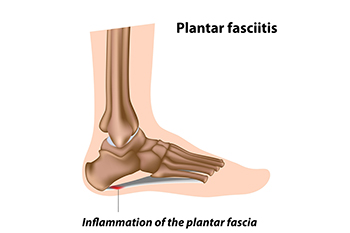
Plantar fasciitis is believed to be the most common complaint of heel pain. Plantar fasciitis is the inflammation of the plantar fascia, a broad band of tissue on the sole that supports the arch. This inflammation can make your heel hurt, swell, or turn red, particularly when getting out of bed in the morning. The causes of plantar fasciitis are varied, often stemming from factors like foot and calf tightness, weak foot muscles, or undue stress on the arch. Excessive running, wearing poorly fitted shoes, and some work actions can make the condition worse. Treatment focuses on addressing the root causes and reducing inflammation. It may involve wearing shoes with better arch support, changing shoe size, and moderating activities that strain the foot. Stretching and strengthening exercises, like towel curls, may help reduce symptoms. If you have developed plantar fasciitis, it is suggested that you make an appointment with a podiatrist who specializes in managing this condition.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Edward Sharrer, DPM from Premier Foot and Ankle Clinic. Our podiatrist can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in North Little Rock, AZ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
Insights Into Hammertoe Surgery

Hammertoe surgery is a procedure aimed at correcting a common and often painful foot condition known as hammertoe. This condition causes one or more toe joints to become permanently bent, resembling a hammer. If conservative treatments fail to provide relief, foot surgery may be recommended. Hammertoe surgery comes in different forms, including tendon transfers, joint resections, and fusion, tailored to the severity and type of deformity. It is typically performed as an outpatient procedure, allowing patients to return home on the same day. Recovery time can vary, and patients can expect swelling and discomfort for a few weeks, with full recovery taking several months. Hammertoe surgery boasts a high success rate in relieving pain and correcting toe deformities. However, understanding the facts about hammertoe surgery is the first step towards making an informed decision about your foot health. If you have a hammertoe, it is strongly suggested that you are under the care of a podiatrist who can determine if this type of foot surgery is correct for you.
Foot surgery is sometimes necessary to treat a foot ailment. To learn more, contact Edward Sharrer, DPM of Premier Foot and Ankle Clinic. Our podiatrist will assist you with all of your foot and ankle needs.
When Is Surgery Necessary?
Foot and ankle surgery is generally reserved for cases in which less invasive, conservative procedures have failed to alleviate the problem. Some of the cases in which surgery may be necessary include:
- Removing foot deformities like bunions and bone spurs
- Severe arthritis that has caused bone issues
- Cosmetic reconstruction
What Types of Surgery Are There?
The type of surgery you receive will depend on the nature of the problem you have. Some of the possible surgeries include:
- Bunionectomy for painful bunions
- Surgical fusion for realignment of bones
- Neuropathy decompression surgery to treat nerve damage
Benefits of Surgery
Although surgery is usually a last resort, it can provide more complete pain relief compared to non-surgical methods and may allow you to finally resume full activity.
Surgical techniques have also become increasingly sophisticated. Techniques like endoscopic surgery allow for smaller incisions and faster recovery times.
If you have any questions please feel free to contact our office located in North Little Rock, AZ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Foot Surgery
In most cases, foot surgery is often chosen as the last available option for conditions that have otherwise been unsuccessfully treated. Surgery may be necessary for several reasons, including the removal of foot deformities (e.g. bone spurs or bunions), arthritis problems, reconstruction due to injury, and congenital malformations (e.g. club foot or flat feet). Regardless of one’s age, foot surgery may be the only successful option for treatment for certain conditions.
The type of surgery one undergoes depends on the type of foot condition the patient has. For the removal of a bunion growth, a bunionectomy is necessary. If the bones in the feet need to be realigned or fused together, a surgical fusion of the foot is needed. For pain or nerve issues, a patient may require surgery in which the tissues surrounding the painful nerve are removed. Initially, less invasive treatments are generally attempted; surgery is often the last measure taken if other treatments are unsuccessful.
While in many cases surgery is often deemed as the final resort, choosing surgery comes with certain benefits. The associated pain experienced in relation to the particular condition is often relieved with surgery, allowing patients to quickly resume daily activities. The greatest benefit, however, is that surgery generally eliminates the problem immediately.
Podiatry history has shown that foot treatments continue to evolve over time. In the field of foot surgery, endoscopic surgery is just one of the many advanced forms of surgery. As technology vastly improves so too will the various techniques in foot surgery, which already require smaller and smaller incisions with the use of better and more efficient tools. Thanks to such innovations, surgery is no longer as invasive as it was in the past, allowing for faster and easier recoveries.